Depression signs and symptoms: How to Recognise Depression & Get Help
By ViaClari Voice | Updated on 3 June, 2025

Depression often begins quietly, with a constant heaviness, persistent fatigue, and a growing disconnection from things that once brought joy. These are more than just low moods; they’re early signs and symptoms of depression, a complex mental health condition that affects how you think, feel, and function. Major depressive disorder doesn’t always announce itself loudly. Sometimes it manifests as restlessness, irritability, or even unexplained physical aches that persist without resolution.
In this blog, we will explain the signs and symptoms of depression in detail. We will cover the emotional, cognitive, physical, and behavioural changes that often signal the onset of major depressive disorder. You will also learn about the possible causes of depression, who may be most at risk, and the treatment options available. Whether you are looking for clarity about your own experience or supporting someone else, this guide offers practical information to help you understand depression and take the next step towards getting help.
🧩 9 Depression Signs and Symptoms
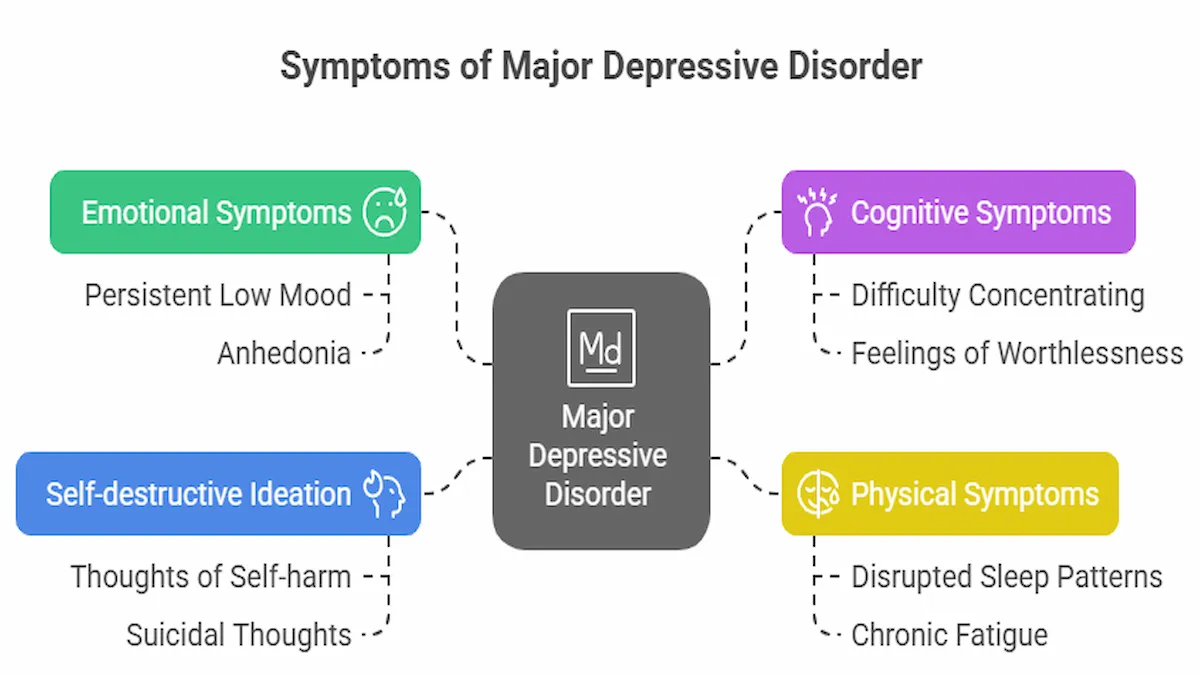
Major depressive disorder can manifest in emotional, cognitive, and physical ways. Recognising the signs is a decisive first step toward getting help. Common symptoms include:
- Persistent low mood — feeling empty, hopeless, or tearful most days
- Anhedonia — loss of interest or pleasure in activities you once enjoyed
- Disrupted sleep patterns — insomnia or sleeping excessively
- Changes in appetite or weight — eating too much or too little
- Chronic fatigue or low energy — even small tasks feel overwhelming
- Feelings of worthlessness or excessive guilt — often irrational or disproportionate
- Cognitive impairment — difficulty concentrating or making decisions
- Physical symptoms — such as headaches, digestive issues, muscle tension, or unexplained aches
- Self-destructive Ideation — Thoughts of self-harm or suicide in severe cases
These symptoms may vary in intensity and duration. For a diagnosis of major depressive disorder, your symptoms typically need to persist for at least two weeks, and they must interfere with your ability to function in work, relationships, or daily routines.
📌 Even if you only relate to a few of these symptoms, your experience is valid. Depression doesn’t need to check every box to be real or worthy of care.
😔 Depression vs. Sadness: A Crucial Distinction
Everyone sometimes feels sad from disappointing events like a breakup, stressful life events, or grieving a loss. Sadness is a normal emotional response. Depression, however, is a mood disorder that affects your overall emotional, mental, and even physical state. Here is a breakdown of key differences:
| Depression | Sadness |
|---|---|
| May develop without a specific cause | Triggered by a clear event |
| Lasts weeks or months | Temporary |
| Interferes with daily life | Doesn't usually affect daily functioning |
| Joy or pleasure in activities you once enjoyed feels absent. | You can still enjoy some things. |
| May worsen without treatment | Improves with time |
💡 If you feel like you’re “not yourself” for an extended period and daily life feels overwhelming or meaningless, it might be more than just sadness, and seeking professional support is essential.
💬 Physical Symptoms That Are Often Overlooked
One of the more surprising elements of depression is how much it can affect the body. Many people first notice physical symptoms of depression before recognising emotional ones. These can include:
- Muscle aches and joint pain
- Stomach issues such as nausea, bloating, or irritable bowel syndrome (IBS)
- Headaches or migraines
- Weight gain or loss unrelated to diet
- Low libido or sexual dysfunction
- Persistent fatigue that doesn’t improve with rest
These symptoms stem from the way depression impacts the brain’s neurotransmitters, including serotonin and dopamine, which are the chemicals that influence both mood and physical processes like pain perception and digestion. Researchers have found that somatic symptoms such as fatigue and gastrointestinal distress in depression are linked to serotonin dysregulation and inflammatory processes in the central nervous system.
🧬 Depression is a medical condition, not a weakness. If your body feels off and no clear physical cause can be found, it’s worth exploring whether mental health could be playing a role.
🧠 How Depression Affects You: Mental, Physical, and Behavioural Impacts
Depression is not just an emotional struggle; it’s a full-body experience that can alter how you think, feel, behave, and function. We know from research that major depressive disorder is associated with functional changes in key brain regions, particularly those involved in emotion regulation and stress response, including the prefrontal cortex and amygdala. Whether it’s the constant fatigue, a foggy mind, or retreating from loved ones, the effects ripple through every part of daily life.
💭 Impacts On Mental Health
Living with depression often feels like being trapped in your own mind. Emotional and cognitive symptoms can include:
- Persistent negative thinking patterns and rumination
- A sense of hopelessness or helplessness about the future
- Trouble concentrating, remembering, or making decisions
- Low self-esteem and feelings of inadequacy or failure
- Loss of motivation for even simple tasks like showering or replying to texts
- Emotional numbness, irritability, or increased anxiety
When left unaddressed, these symptoms can strain relationships, disrupt careers, and affect your ability to engage with the world. Depression can also increase the risk of developing other mental health concerns, such as anxiety disorders or eating disorders.
🧍♀️ Impacts On Physical Health
Depression doesn’t only live in the mind; it also affects the body in powerful and sometimes confusing ways. These physical symptoms are just as real and impactful:
- Muscle pain or tension
- Digestive issues like IBS, nausea, or bloating
- Frequent headaches or migraines
- Changes in appetite and weight
- Chronic fatigue that rest doesn’t fix
- Sleep disruptions, either insomnia or oversleeping
- Sexual health issues, including low libido
These symptoms arise because depression alters the activity of neurotransmitters like serotonin and dopamine, which regulate both emotional well-being and physical functions like digestion, pain response, and energy levels. Researchers have found that somatic symptoms are not just secondary effects but integral parts of depressive episodes, particularly in patients with chronic depression.
📌 If your body feels “off” and no physical cause is found, it’s worth exploring your mental health as a contributing factor.
🚬 Impacts on Behavioural Health
To cope with the mental and physical weight of depression, some people may turn to substances. While alcohol, recreational drugs, or prescription misuse may offer temporary relief, they typically worsen symptoms over time. Studies show that co-occurring depression and substance use disorders are associated with poorer treatment outcomes, including higher relapse rates and more severe symptomatology.
Depression-related substance use can:
- Interfere with the effectiveness of antidepressants
- Increase mood swings and emotional instability
- Heighten feelings of shame, guilt, or isolation
- Deepen dependency cycles that make recovery harder
This is why dual diagnosis support, treating both depression and substance use together, is crucial for those struggling with both.
🧬 Depression Affects the Whole Person, and So Should Healing
Mental, physical, and behavioural symptoms are all interconnected. Addressing just one area (like sleep or sadness) without considering the others may delay healing. A holistic approach, encompassing therapy, medical care, and lifestyle support, provides the most effective path forward.
💡 You’re Not Alone 💡
If you’re reading this and recognising yourself in these words, take heart.
Millions of people live with depression, and many recover with the right support. It’s okay to ask for help. In fact, it’s one of the bravest steps you can take.
🧬 What Causes Depression, and Who Is at Risk?
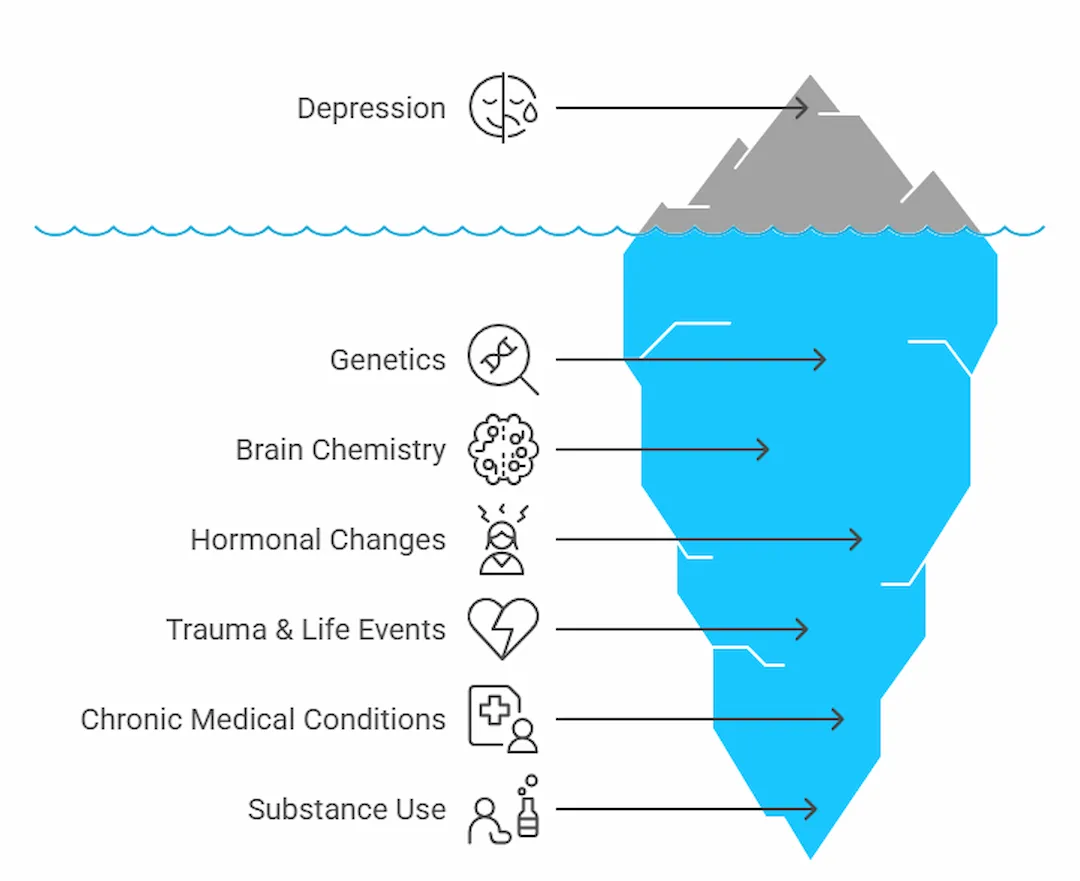
Depression is rarely the result of a single event or issue. Instead, it usually arises from a complex interplay of causes and risk factors, including biology, environment, life events, and personal history. Understanding what contributes to depression can reduce shame and provide a clearer path toward healing.
🔍 Key Causes of Depression
While each individual’s experience with depression is unique, some of the most well-established causes include:
- Genetics: If you have a close family member with depression or another mood disorder, your own risk increases. Inherited traits may affect how your brain regulates mood and stress. We know from large-scale genome-wide studies that major depressive disorder has a heritable component, with identified risk loci influencing mood regulation and stress reactivity.
- Brain chemistry imbalances: Neurotransmitters like serotonin, dopamine, and norepinephrine play a crucial role in mood regulation. When these chemicals are out of balance, it can lead to symptoms of depression.
- Hormonal changes: Hormonal shifts can significantly influence mood. Perinatal and postpartum depression, premenstrual dysphoric disorder (PMDD), and depression during menopause are all examples of hormone-related mood disturbances.
- Trauma and major life events: Childhood abuse, neglect, loss of a loved one, financial instability, divorce, or job loss can all act as powerful emotional triggers, especially if the trauma remains unresolved.
- Chronic medical conditions: Illnesses such as diabetes, cancer, heart disease, thyroid disorders, or chronic pain can directly contribute to or worsen depression. These physical conditions can take a toll on both the emotional and neurological levels.
- Substance use: Alcohol, recreational drugs, and even the misuse of prescription medication can disrupt brain chemistry and deepen depressive episodes. Substance use may sometimes begin as a coping strategy but evolve into a contributing factor.
📌 Important: You don’t need a dramatic “reason” to feel depressed. Sometimes, depression develops without any obvious cause, and that doesn’t make it any less valid or worthy of treatment.
⚠️ Understanding Risk Factors: Who Is Most Vulnerable?
While depression can affect anyone, certain people are at greater risk due to overlapping biological and psychosocial factors. Risk factors don’t guarantee depression will occur, but they do increase vulnerability.
Here are some of the most common risk factors:
- Personal history of depression or anxiety
Previous episodes increase the likelihood of future ones, especially if left untreated. - Family history of mental health disorders
Genetics and family dynamics both play a role. - Early childhood trauma or neglect
Adverse childhood experiences (ACEs) can have profound and lasting impacts on brain development and emotional regulation. We know from longitudinal studies that adverse childhood experiences significantly heighten the risk of adult depression by disrupting emotional regulation pathways and stress responses. - Ongoing stress and adversity
Chronic financial hardship, caregiving burdens, job instability, or abusive relationships can all wear down mental resilience over time. - Social isolation or lack of support
People with weak social ties or limited access to supportive relationships are more prone to depression. - Belonging to a stigmatised or marginalised group
Discrimination based on race, gender, sexual orientation, disability, or immigration status can contribute to chronic stress and depressive symptoms. - Substance misuse
Not only a cause but also a risk factor. Regular use of alcohol or drugs can trigger or worsen existing depression. - Age-specific risks
- Teens may show irritability, low motivation, or academic decline rather than sadness.
- Older adults may experience depression that’s mistaken for “just ageing,” especially when symptoms appear as fatigue, memory loss, or physical complaints.
🧬 How Health Conditions Can Contribute to Depression
Certain medical issues can directly lead to or exacerbate depression:
| Health Condition | Connection to Depression |
|---|---|
| Thyroid imbalances | Can mimic or trigger depressive symptoms |
| Heart disease | Often linked with post-illness emotional struggles. |
| Chronic pain | Increases the risk of developing depression |
| Neurological disorders | Conditions like Parkinson’s or MS can affect mood. |
| Hormonal changes | Can lead to perinatal or postpartum depression |
Chronic health issues like diabetes and cardiovascular disease are not only physically taxing but have been shown to double the risk of developing depressive symptoms over time. If you’ve been diagnosed with a chronic illness, be aware of your mood and don’t hesitate to speak up if you’re struggling emotionally as well.
🧠 Takeaway: Understanding your unique risk factors helps you prevent or manage depression and empowers you to seek support early before symptoms escalate.
The good news is that depression, no matter the cause, is highly treatable. With a wide range of therapies and tools available, recovery is not only possible; it’s probable.
💊 How Can Depression Be Treated?

Depression is highly treatable. With the right treatment plan, most people experience significant improvement in their symptoms and overall function. There’s no one-size-fits-all approach, and that’s a good thing. Whether you’re experiencing mild, moderate, or severe depression, there are various effective treatments for depression to explore.
1.🌿Talking Therapies
Talking therapies can make a huge difference, offering a safe, non-judgmental space to explore thoughts, feelings, and patterns.
Popular and effective options include:
- Cognitive Behavioural Therapy (CBT) – Helps to challenge and reframe negative thinking habits.
- Interpersonal Therapy (IPT) – Focuses on improving communication and strengthening relationships.
- Psychodynamic Therapy – Explores how past experiences may influence current emotions and behaviours.
These therapies can be accessed face-to-face, over the phone, or online — whatever feels right for you.
2.💊 Medications
Antidepressants can be a valuable part of treatment, especially for people with moderate to severe depression or depression and anxiety together.
There are several types, including:
- SSRIs (e.g. sertraline, fluoxetine)
- SNRIs (e.g. venlafaxine)
- Tricyclics (older, used less often due to side effects)
Antidepressants are proven to be very effective in treating depression. A meta-analysis of clinical trials revealed that selective serotonin reuptake inhibitors (SSRIs) are significantly more effective than placebo in treating moderate to severe depression.
It’s completely understandable to feel cautious about medication. But it’s worth noting:
- They are not addictive
- They may take 2–4 weeks to work
- Side effects usually settle after the first few weeks
Always discuss the pros and cons with your GP or mental health provider. Medication is most effective when used in conjunction with therapy and lifestyle modifications. It’s not a cure-all, but it can be a powerful part of the puzzle.
3. 🚀 Advanced Options
For some, especially when symptoms don’t improve with initial treatments, advanced interventions may be explored. This can include:
- Referral to a psychiatrist for specialist input
- Intensive therapy programmes
- In certain cases, options like electroconvulsive therapy (ECT) may be considered
These are always tailored and closely monitored by professionals to ensure safety and effectiveness.
Of course, finding the right treatment can feel overwhelming, and that’s where professional guidance becomes invaluable.
🧑⚕️ Working with a Mental Health Professional to Treat Depression
Navigating treatment options can feel overwhelming. That’s why working with a professional, whether a GP, psychologist, psychiatrist, or counsellor, is so crucial.
They can help:
- Identify the type of depression you’re experiencing
- Create a tailored treatment plan
- Monitor your progress and make adjustments as needed
- Offer guidance on lifestyle strategies to prevent depression from recurring
And remember, seeking help is not a sign of weakness. It’s an act of self-awareness and strength 💪
💡 There Is a Way Through 💡
You are not your diagnosis.
Depression may shape your days right now, but it doesn’t define who you are or who you can become.
With support, healing is possible. And it begins with understanding your options.
.
🆘 How Do You Get Help for Depression?
So far, we’ve explored what depression feels like, what causes it, and the many ways it can be treated. But here’s the big question:
👉 What should you actually do if you think you’re experiencing depression?
Whether you’re in the midst of a depressive episode or quietly wondering if something feels “off,” reaching out is not only wise, but it’s also the first step to feeling better.
So, where do you begin? Whether you’re seeking support for the first time or looking to adjust your current approach, here are some clear steps you can take.
🪜 Steps to Take if You Experience Depression
If you’ve noticed changes in your mood, energy, or motivation, don’t wait for things to get worse. Here’s what you can do:
1. Talk to Someone You Trust
Open up to a friend, family member, colleague, or partner. You don’t have to have all the words. Just saying “I haven’t been feeling like myself” is enough.
2. Book a GP Appointment
Your GP is a great place to start. They can:
- Provide a preliminary diagnosis
- Rule out physical causes (e.g. thyroid issues)
- Refer you to mental health services
- Discuss treatment options like therapy or antidepressants
3. Track Your Mood and Symptoms
Jotting down how you’re feeling each day, including sleep, appetite, mood, and energy, can help both you and your healthcare provider understand what’s going on.
4. Limit Alcohol and Drugs
It’s common for people with depression to turn to substances as a way to cope, but this usually worsens symptoms. Substance use and depression often fuel each other in a vicious cycle.
5. Don’t Self-Diagnose, But Do Take Yourself Seriously
Reading online can be helpful (hello 👋), but it’s not a substitute for personalised support. If you suspect you might have clinical depression, don’t wait for it to “go away on its own.” Get the help you deserve.
📚 Resources for People Diagnosed with Depression
Support is out there, and you don’t have to face depression alone 🌍. Whether you’re in the UK, the US, or anywhere else, there are trusted organisations offering help, many of them free or low-cost.
From 24/7 crisis lines to therapy services, you’ll find resources tailored to different needs, including youth support, culturally sensitive care, and men’s mental health initiatives.
💡 You can often self-refer, and many services now offer online, phone, or in-person options — whatever suits your comfort and situation.
👉 For country-specific crisis and mental health resources, visit our global support directory.
Help is closer than you think, and reaching out is a powerful first step.
You matter. You are not a burden. And you are not alone.
🚨 When to Seek Immediate Treatment for Severe Depression
If you or someone you love is showing signs of severe depression, it’s vital to take it seriously. Signs to watch for include:
- Thoughts of self-harm or suicide
- Not being able to function at all (e.g. getting out of bed, washing, eating)
- Sudden withdrawal from life or relationships
- Losing touch with reality (psychotic symptoms, hearing voices, etc.)
🆘 Don’t wait. Get urgent help by:
- Calling your GP for an emergency appointment
- Contacting emergency services in your country if there is a threat to your life
- Going to your nearest A&E department
- Reaching out to a crisis help line
👉 For emergency support options in your country, visit our global support directory.
You matter. You are not a burden. And you are not alone.
💬Final Thoughts: Living with Depression and Finding Hope 🌱
Depression can feel isolating, but you are never alone. It’s a treatable condition, and with the right support, healing is absolutely possible. Whether you’re facing it yourself or supporting someone close to you, know that things can get better.
Taking that first step, even just reading this, is already an act of courage. 💙
💡 Ready to Take the Next Step?
Reach out to your GP, speak to a therapist, or explore trusted resources.
There’s help. There’s hope. And there’s a future waiting for you — one step at a time.
🙋♀️ FAQ: Understanding Depression in Depth
What is depression, and how is it classified as a mental disorder?
Depression is a mental disorder that affects the way you feel, think, and act. It’s classified as a mood disorder that causes a persistent feeling of sadness and loss of interest in daily activities. It’s not just a passing mood. It’s a serious condition that requires attention and care.
What are the common depression symptoms I should watch for?
Depression symptoms may include low mood, fatigue, changes in sleep or appetite, loss of interest in activities, difficulty concentrating, and feelings of guilt or hopelessness. Severe symptoms can even lead to thoughts of self-harm or suicide.
How is depression diagnosed by professionals?
To diagnose depression, a healthcare provider will evaluate your symptoms, medical history, and daily functioning. The diagnosis of depression typically requires that symptoms occur most of the day, nearly every day, for at least two weeks.
What causes depression, and who is at risk?
Depression can stem from many factors, like genetics, brain chemistry, trauma, or chronic stress, which may all play a role in depression. Women are more likely to experience it, and children and adolescents are also at risk. Life changes, hormonal shifts, and certain medications can also contribute to these changes.
What is major depression?
Major depression (or major depressive disorder) is a form of depression that causes a persistent feeling of sadness and a lack of interest in life. It’s one of the most common mental health conditions worldwide and can severely affect work, relationships, and well-being.
What’s the link between substance abuse and mental health?
There’s a strong connection between substance abuse and mental health. People with depression may turn to alcohol or drugs, which can make symptoms worse. So it is essential to seek resources that offer support for those needing dual treatment.
Can seasonal depression affect anyone?
Yes, seasonal depression (also known as seasonal affective disorder) is triggered by changes in daylight, most commonly in winter. It causes symptoms similar to depression, including low mood, lethargy, and difficulty concentrating.
What is premenstrual dysphoric disorder (PMDD)?
PMDD is a severe form of premenstrual syndrome. It’s a mood disorder that causes intense mood swings, irritability, and symptoms similar to depression in the weeks leading up to menstruation.
Can children get depression?
Absolutely. Depression in children and teens is real, although symptoms may include irritability and school refusal rather than sadness. Depression can happen at any age, and early intervention is key.
What’s the outlook for people with depression?
The majority of people with depression improve with treatment. While depression is a serious condition, it can be treated, and most individuals eventually respond well to treatment, especially with a combination of therapy and medication.
Is treatment always necessary, even for mild cases?
Yes, even mild depression can worsen without treatment. Treatment may include therapy, lifestyle changes, or medication. It’s essential to receive treatment early to prevent further escalation.
How is depression different from general sadness or anxiety?
While everyone feels low from time to time, depression is different. It’s persistent, overwhelming, and often has no clear cause. It can also co-occur with anxiety and depression symptoms, complicating the experience.
Can you experience symptoms of depression and not be depressed?
Yes, short-term symptoms usually follow stressful life events, like grief. However, if symptoms begin to affect your daily life and don’t improve, it could signal depression at some point and should be discussed with a professional.
